Osteoporosis, often referred to as a “silent disease,” affects hundreds of millions of women globally—yet most are unaware until a bone fracture occurs. Characterized by low bone mass and deteriorating bone tissue, osteoporosis in women is far more common than in men, especially after menopause. This medically-reviewed guide explores the causes, symptoms, prevention strategies, and treatments for osteoporosis in women, with a focus on postmenopausal health, diet, and diagnostic tests.
What Is Osteoporosis?
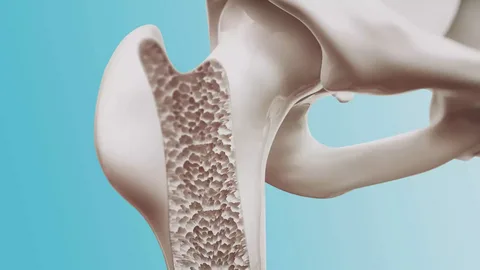
Osteoporosis is a condition where bones become porous, fragile, and prone to fractures, usually without any preceding symptoms. Over time, this leads to a significant loss in bone mineral density (BMD) and overall skeletal strength.
Why Are Women at Higher Risk?
Women are at significantly greater risk than men due to biological, hormonal, and lifestyle factors. According to the International Osteoporosis Foundation, up to 1 in 3 women over 50 will suffer an osteoporosis-related fracture.
Key Reasons Women Are More Affected:
-
Smaller and thinner bones compared to men
-
Estrogen drop during menopause, accelerating bone loss
-
Longer life expectancy means more years at risk
-
Pregnancy & breastfeeding deplete calcium stores
Osteoporosis and Menopause
Estrogen plays a crucial role in maintaining bone density. During menopause, estrogen levels drop sharply, triggering rapid bone loss. Women can lose up to 20% of their bone mass within 5–7 years post-menopause. Important: Bone loss can begin as early as perimenopause, making early screening essential.
Symptoms of Osteoporosis in Women
Early osteoporosis has no symptoms, and most women don’t realize they have it until a fracture occurs.
When symptoms appear:
-
Back pain from vertebral fractures
-
Loss of height
-
Stooped posture (kyphosis or “dowager’s hump”)
-
Fractures from simple actions (bending, coughing, tripping)
-
Bone pain or tenderness
Causes of Osteoporosis in Women
Primary Causes & Their Impact on Bone Health:
| Cause | How It Affects Bone Health |
|---|---|
| Hormonal changes | Menopause & estrogen deficiency |
| Ageing | Natural bone loss accelerates with age |
| Nutritional deficiency | Low calcium & vitamin D weaken bones |
| Sedentary lifestyle | Lack of weight-bearing exercise lowers BMD |
| Smoking & alcohol | Interfere with calcium absorption |
| Genetics | Family history increases risk |
| Chronic diseases | Thyroid issues, celiac disease, rheumatoid arthritis |
| Medications | Long-term steroid & anticonvulsant use |
Osteoporosis Risk Factors in Women
You may be at risk if you:
-
Are over 50 or postmenopausal
-
Have a family history of osteoporosis
-
Have had a previous fracture
-
Are underweight or have an eating disorder
-
Have vitamin D deficiency
-
Smoke or drink excessively
-
Take corticosteroids regularly
-
Live a sedentary lifestyle
Bone Density Test for Women
The most reliable diagnostic tool is Dual-Energy X-ray Absorptiometry (DEXA/DXA scan), measuring bone mineral density in the hip and spine.
Recommended Screening:
-
All women over 65
-
Postmenopausal women under 65 with risk factors
-
Women with a history of fractures
How to Prevent Osteoporosis in Women
Top prevention strategies:
-
Calcium: 1,200 mg/day for women over 50
-
Vitamin D: Sunlight or supplements
-
Weight-bearing exercises: Walking, dancing, resistance training
-
Quit smoking & limit alcohol
-
Avoid crash diets & nutrient deficiencies
-
Prevent falls at home (install railings, remove clutter)
Osteoporosis Diet for Women
Foods That Support Bone Health:
| Nutrient | Best Sources |
|---|---|
| Calcium | Dairy, leafy greens, almonds, sesame |
| Vitamin D | Sunlight, fortified milk, fatty fish |
| Magnesium | Pumpkin seeds, avocados, spinach |
| Protein | Eggs, tofu, lentils, lean meats |
| Vitamin K2 | Natto, eggs, hard cheeses |
| Zinc | Chickpeas, nuts, whole grains |
| Avoid excessive caffeine, soda, and salty processed foods. |
Best Supplements for Osteoporosis in Women
When diet & sunlight aren’t enough:
-
Calcium carbonate or citrate
-
Vitamin D3 (cholecalciferol)
-
Magnesium with vitamin B6
-
Vitamin K2 (MK-7 form)
-
Collagen or strontium (advanced cases)
Always consult a doctor before starting supplements.
Osteoporosis Treatment: Medical Options for Women
| Drug Class | Examples | Effect |
|---|---|---|
| Bisphosphonates | Alendronate, Risedronate | Slow bone loss |
| SERMs | Raloxifene | Mimic estrogen to protect bones |
| Parathyroid Hormone | Teriparatide (Forteo) | Stimulates bone formation |
| Monoclonal Antibodies | Denosumab | Prevents bone breakdown |
| Hormone Therapy | Estrogen (select cases) | Used for younger postmenopausal women |
Living with Osteoporosis: Tips for Safer, Stronger Living
-
Exercise safely to maintain balance & strength
-
Modify your home to reduce fall risks
-
Get regular check-ups & BMD scans
-
Stay consistent with medication & nutrition
-
Join support groups or education programs
Conclusion
Osteoporosis in women is often silent until it’s too late. But awareness, early testing, and proactive steps can preserve bone health well into old age. Whether you’re 30, 50, or 70, it’s never too early—or too late—to build stronger bones.
FAQs About Osteoporosis in Women
At what age should women worry about osteoporosis? Women should begin preventive steps in their 30s; regular screening is recommended after 50.
Is osteoporosis reversible? Bone mass can’t be fully restored, but progression can be slowed, reducing fracture risk.
Can young women get osteoporosis? Yes, especially those with eating disorders, hormonal issues, or long-term steroid use.
How is osteoporosis diagnosed? Through a DEXA scan measuring bone mineral density.
What is the best exercise for osteoporosis? Weight-bearing activities like brisk walking, resistance training, and balance exercises (tai chi, yoga).
Read More: Signs and Symptoms of Vitamin D Deficiency


60 Comments
It’s best to participate in a contest for among the best blogs on the web. I’ll advocate this site!
A lot of thanks for your entire effort on this website. Debby takes pleasure in participating in internet research and it’s really simple to grasp why. My partner and i know all relating to the lively medium you make informative solutions via your blog and in addition inspire contribution from others on the concern and my girl is always being taught a lot. Enjoy the remaining portion of the new year. You are always carrying out a superb job.
I liked as much as you will receive performed right here. The comic strip is tasteful, your authored material stylish. however, you command get bought an shakiness over that you wish be delivering the following. ill without a doubt come more previously again as exactly the similar just about very regularly within case you shield this increase.
You are my intake, I own few blogs and often run out from to post .
Oh my goodness! an amazing article dude. Thanks Nevertheless I’m experiencing problem with ur rss . Don’t know why Unable to subscribe to it. Is there anyone getting identical rss problem? Anyone who knows kindly respond. Thnkx
Of course, what a fantastic website and educative posts, I will bookmark your website.Best Regards!
Outstanding post, you have pointed out some great points, I also conceive this s a very great website.
We’re a group of volunteers and opening a new scheme in our community. Your website provided us with valuable information to work on. You’ve done an impressive job and our entire community will be grateful to you.
There are certainly quite a lot of details like that to take into consideration. That may be a great level to deliver up. I offer the ideas above as common inspiration however clearly there are questions like the one you bring up where crucial factor might be working in sincere good faith. I don?t know if finest practices have emerged around things like that, but I am positive that your job is clearly recognized as a fair game. Both girls and boys really feel the impact of only a moment’s pleasure, for the rest of their lives.
This design is wicked! You most certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
I believe this site contains some very excellent information for everyone. “A sense of share is not a bad moral compass.” by Colin.
Hello. remarkable job. I did not imagine this. This is a splendid story. Thanks!
Can I simply say what a relief to find somebody who really is aware of what theyre speaking about on the internet. You positively know easy methods to carry a problem to light and make it important. More people must learn this and understand this side of the story. I cant consider youre not more popular since you undoubtedly have the gift.
Thanks on your marvelous posting! I quite enjoyed reading it, you’re a great author.I will be sure to bookmark your blog and will often come back sometime soon. I want to encourage continue your great writing, have a nice day!
It’s actually a nice and useful piece of info. I’m happy that you just shared this useful information with us. Please stay us informed like this. Thank you for sharing.
What i do not realize is actually how you’re not actually much more well-liked than you may be right now. You are very intelligent. You realize therefore significantly relating to this subject, made me personally consider it from so many varied angles. Its like men and women aren’t fascinated unless it is one thing to accomplish with Lady gaga! Your own stuffs outstanding. Always maintain it up!
Very nice post. I just stumbled upon your blog and wanted to say that I have truly enjoyed browsing your blog posts. In any case I will be subscribing to your feed and I hope you write again very soon!
As soon as I detected this site I went on reddit to share some of the love with them.
I am glad to be a visitor of this utter website! , appreciate it for this rare info ! .
But wanna remark on few general things, The website style and design is perfect, the written content is really superb. “Art for art’s sake makes no more sense than gin for gin’s sake.” by W. Somerset Maugham.
Hello, you used to write great, but the last several posts have been kinda boring?K I miss your super writings. Past several posts are just a little out of track! come on!
Saved as a favorite, I really like your blog!
I went over this web site and I believe you have a lot of good information, saved to my bookmarks (:.
Thanks a bunch for sharing this with all of us you really know what you’re talking about! Bookmarked. Please also visit my web site =). We could have a link exchange agreement between us!
In the great scheme of things you’ll receive a B+ with regard to effort and hard work. Where exactly you confused me ended up being on your specifics. You know, they say, the devil is in the details… And it could not be much more true here. Having said that, allow me inform you what did work. The text can be quite engaging which is probably why I am taking the effort in order to comment. I do not make it a regular habit of doing that. Next, despite the fact that I can see a leaps in reasoning you come up with, I am not really confident of how you appear to connect the details which in turn make the actual final result. For now I will yield to your point however trust in the foreseeable future you link the facts much better.
I do not even know how I ended up here, but I thought this post was good. I don’t know who you are but certainly you’re going to a famous blogger if you are not already 😉 Cheers!
I am impressed with this web site, real I am a fan.
Attractive portion of content. I just stumbled upon your site and in accession capital to assert that I acquire actually loved account your weblog posts. Anyway I will be subscribing on your augment or even I achievement you get right of entry to consistently rapidly.
WONDERFUL Post.thanks for share..more wait .. …
Do you have a spam issue on this site; I also am a blogger, and I was wondering your situation; many of us have created some nice procedures and we are looking to exchange solutions with others, please shoot me an e-mail if interested.
I wanted to thank you for this great read!! I definitely enjoying every little bit of it I have you bookmarked to check out new stuff you post…
I’ve recently started a site, the information you provide on this website has helped me greatly. Thank you for all of your time & work.
Hi there, simply was aware of your blog via Google, and located that it’s truly informative. I am gonna be careful for brussels. I’ll appreciate if you happen to proceed this in future. Many people will likely be benefited out of your writing. Cheers!
Some really great articles on this site, thanks for contribution.
I think this internet site has very great pent subject matter blog posts.
I am no longer sure the place you are getting your info, but good topic. I needs to spend a while studying much more or working out more. Thanks for fantastic info I used to be searching for this info for my mission.
I conceive this website contains some rattling good info for everyone :D. “Years wrinkle the skin, but to give up enthusiasm wrinkles the soul.” by Samuel Ullman.
Great work! This is the type of information that should be shared around the net. Shame on the search engines for not positioning this post higher! Come on over and visit my web site . Thanks =)
I was looking through some of your posts on this site and I believe this web site is very instructive! Continue putting up.
Those are yours alright! . We at least need to get these people stealing images to start blogging! They probably just did a image search and grabbed them. They look good though!
I do not even know how I ended up here, but I thought this post was great. I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
You are my inspiration , I own few blogs and very sporadically run out from to brand.
It’s actually a great and helpful piece of info. I’m satisfied that you shared this helpful info with us. Please keep us up to date like this. Thank you for sharing.
Hi, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you stop it, any plugin or anything you can suggest? I get so much lately it’s driving me crazy so any help is very much appreciated.
you have a great blog here! would you like to make some invite posts on my blog?
I am glad to be one of several visitors on this great web site (:, thankyou for posting.
It is truly a nice and helpful piece of info. I’m glad that you simply shared this helpful info with us. Please stay us up to date like this. Thank you for sharing.
Hey There. I found your blog using msn. This is an extremely well written article. I’ll make sure to bookmark it and come back to read more of your useful info. Thanks for the post. I will definitely return.
Very good written information. It will be useful to anybody who utilizes it, as well as yours truly :). Keep doing what you are doing – looking forward to more posts.
As I web site possessor I believe the content material here is rattling wonderful , appreciate it for your hard work. You should keep it up forever! Good Luck.
Fantastic site. Plenty of useful information here. I am sending it to a few friends ans also sharing in delicious. And naturally, thanks for your sweat!
I went over this website and I believe you have a lot of good info, saved to favorites (:.
I haven’t checked in here for some time because I thought it was getting boring, but the last few posts are great quality so I guess I will add you back to my daily bloglist. You deserve it my friend 🙂
Thank you for any other excellent post. Where else could anybody get that type of info in such a perfect manner of writing? I have a presentation next week, and I’m on the look for such info.
It’s really a cool and useful piece of information. I am satisfied that you simply shared this useful information with us. Please stay us up to date like this. Thank you for sharing.
I have recently started a blog, the info you provide on this website has helped me greatly. Thanks for all of your time & work.
I used to be very happy to search out this web-site.I needed to thanks in your time for this glorious learn!! I definitely enjoying every little little bit of it and I’ve you bookmarked to take a look at new stuff you weblog post.
Lovely just what I was searching for.Thanks to the author for taking his time on this one.
Everything is very open and very clear explanation of issues. was truly information. Your website is very useful. Thanks for sharing.
Hello there, You’ve done a fantastic job. I will definitely digg it and personally recommend to my friends. I’m confident they’ll be benefited from this web site.